Sitting down with a couple of women I had just met at the airport waiting for a delayed flight turned out to be interesting. We discussed and laughed like old friends who were meeting for a reunion. Our conversations were full of sisterly love and among the many things we discussed, we touched on the issue of menopause, the transition, and the changes it brings to your body which normally has an effect on your mind, specifically your mental health.
The time leading up to menopause (called perimenopause) is a physical and emotional roller coaster for some women. The so-called “change of life” comes with a host of symptoms triggered by hormonal shifts — hot flashes, insomnia, mood fluctuations and even depression.
When women go through sudden hormonal changes like those that come with perimenopause, puberty, postpartum and even their monthly cycle, they’re at a higher risk for depression. The incidence of depression doubles during this time and as funny as it may sound, the women described incidences of uncontrollable crying which cannot even be compared to labour or mourning. At least in labour, you are crying because you are in pain but for menopause, you don’t know why you have a of bucket full of tears ready to be poured out. The women said you can cry over silly small incidences of someone not seasoning the food well or someone serving you in a teacup that you do not like or the bread not having enough butter and I thought to myself that even load-shedding must be taking a toll on most women.
Shifts in the levels of female hormones can cause mood changes at other stages of life, so it’s not necessarily surprising that they can have some effect on mood during the menopausal transition. Premenstrual dysphoric disorder, which is a more severe form of premenstrual syndrome, affecting mood, and postpartum depression are other examples of conditions that are driven by hormonal changes inside the body — in these cases, before menstruation or after childbirth. For women who have struggled in the past with depression or anxiety they might actually see a resurgence in symptoms.
Mood shifts during perimenopause and at menopause are most often mild. The vast majority of women who develop significant mood issues during perimenopause have had them in the past. When menopause occurs — it’s a time when women sometimes face multiple sources of stress, including caring for children, dealing with aging parents, and navigating life changes, all of which may contribute to the incidence of depression and anxiety at this age.
There is some evidence that women are more likely to experience panic attacks during and after the menopausal transition. A panic attack is marked by a sudden sense of extreme anxiety, accompanied by symptoms such as sweating, trembling, shortness of breath, or harmless heart rhythm disturbances called palpitations. During a panic attack, your heart may race and you may feel sweaty and hot. The same is true of hot flashes. Before a hot flash, some women experience an “aura,” which is a term doctors use to describe a sensation preceding a brain condition (such as migraine). For these women, the hot flash is preceded by a panic feeling or a sense of doom. One way to distinguish between hot flashes and panic attacks is that hot flashes don’t make you feel short of breath, while panic attacks may.
Changes in your physical health at the time of menopause may also drive mood changes. For example, anxiety may be triggered by an overactive thyroid gland, which becomes more common with age. In addition, anxiety and depression may be triggered by a lack of sleep, which also becomes more common at the time of menopause, as hormone shifts cause night-time hot flashes or other sleep disruptions that make it more difficult for women to get the rest they need.
So, what can you do to protect your mental health as you go through menopause? Beware of the mood changes that may accompany other menopausal symptoms and monitor your mood by taking note of patterns in other factors such as sleep and stress levels. Seek professional help if symptoms become severe and interfere with daily life. Make lifestyle changes such as increasing exercise, getting adequate sleep, and controlling stress to reduce potential symptoms. Reach out to others so you do not struggle alone.
Menopause is technically one day in a woman’s life that occurs 12 months after her last period. Afterward, women are considered postmenopausal. Before then, you’re in the perimenopause stage when reproductive hormones are shifting and can make you more vulnerable to major depression.
Most of the time, when people are talking about menopause or going through “the change,” they’re actually referring to perimenopause. During this phase, the menstrual cycle becomes irregular — longer, shorter, heavier, lighter, infrequent, or closer together.
The same hormones that control your menstrual cycle also influence serotonin, a brain chemical that promotes feelings of well-being and happiness. When hormone levels drop, serotonin levels also fall, which contributes to increased irritability, anxiety, and sadness.
Falling estrogen and progesterone levels can trigger mood swings that make you less able to cope with things you’d normally let roll off your back. For some, these hormonal dips can set off a depressive episode, especially for those who’ve gone through major depression in the past.
It’s common to experience bouts of insomnia during perimenopause, partly because of night-time hot flashes. Poor sleep can make you up to ten times more likely to become depressed.
Perimenopause typically occurs in your 40s. Turbulent hormones aside, this can also be a stress-filled stage of life with events that impact emotional health, such as:
• Aging parents
• Career pressure
• Health problems
• Kids leaving home
These external pressures can make mood swings worse, as well as trigger or increase depression.
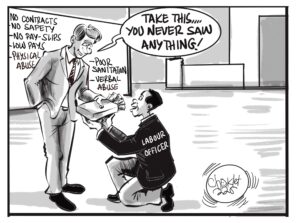
To the Minister of Labour, our appeal as women is that you consider giving women a different option when it comes to retirement age. The current early retirement age is at 55 and normal retirement at 60. External pressures give women mood swings and can trigger depression, be considerate in the Policy making and allow women to have better options to leave earlier if need be because you never know what a woman is going through, mentally and physically.
If you’ve been diagnosed with depression in the past talk to your doctor if your previous symptoms return or if you have new ones, including:
• Persistent feelings of sadness, hopelessness, or irritability
• Low appetite or overeating
• Oversleeping or insomnia
• Overwhelming fatigue and lack of motivation
• Loss of interest in activities previously enjoyed
• Difficulty making decisions and absorbing information
• Thoughts of suicide
If you’re having frequent mood swings or other symptoms of depression that are affecting your life, it’s important to talk to your primary care doctor or obstetrician-gynaecologist. Many symptoms of perimenopause respond well to hormonal medications. An estrogen patch with progesterone pills or a very low-dose oral contraceptive pill may offer relief.
However, taking hormonal medications for depression may not be a good option if you:
• Smoke
• Have high blood pressure
• Have a history of blood clotting problems
• Are postmenopausal
Antidepressants may be helpful for mood symptoms in those who aren’t candidates for hormonal medications and when this treatment is coupled with cognitive behavioural therapy, it is the most effective approach to managing depression.
Lifestyle adjustments can also help reduce perimenopause symptoms and promote good postmenopausal health. Healthy habits include eating a nutritious diet, exercising regularly, and limiting caffeine and alcohol consumption. Reaching menopause can be a relief. Once hormones settle down, mood fluctuations may end.
The good news is that mood fluctuations are treatable. If emotional ups and downs during perimenopause impact your normal daily activities (work, school, hobbies) or your relationships, talk to your doctor about your options.
Shout out to Dr. Maputa, Ms. Mable Mudenda and the other beautiful lady in dreads (whose name I didn’t catch, pardon me) for a conversation that was worth-while!
Seek help when in need, visit a counsellor near you!
About the author
Aka Monde, is a licensed Professional Counsellor who holds a Master of Science in Counselling from the University of Zambia. She believes in the adage “a problem shared, is a problem half solved.” Speak to your pastor, church elder, elderly family member or see a professional counsellor when in need.
Email: [email protected]