In last week’s article we examined the progress that the National Health Insurance Management Authority (NHIMA) has made in the implementation of the National Health Insurance Scheme (NHIS).The NHIS was created and implemented in order to provide universal access to quality health care for all Zambians. It has been operational since October of 2019.
In this article we explore the challenges and bottlenecks that could hinder effective rollout of the NHIS.
In order to understand the limitations in rolling out and implementing universal health care, it is important to have an appreciation for the elements that comprise the concept of universal access. Universal access to healthcare provides a measure of how much a population can reach health services. This is often intertwined with universal coverage which determines the population or beneficiaries that can access a set package of health care benefits.Universal health coverage means that all people have access to the health services they need, when and where they need them, with financial protection from direct payment for health services. (WHO: 2019).In summary, universal health care has three (3) pillars: service delivery, health financing and governance.
A core advantage of universal health care is that ultimately every citizen receives the same level and standard of care, leading to a healthier workforce and increased life expectancy. A further advantage is that administratively, health care provision is managed through one central agency as opposed to a decentralized system.
Making progress towards universal health coverage thus requires governments to strengthen those elements of the health system that make it possible to deliver services of high quality.
Issues that may pose challenges to the NHIS Implementation include:
(i) Co-existence of NHIS with private health care insurance
In a Zambian context, the NHIS is implemented alongside a parallel private and profit-making health care insurance systems. In other words, there exists a dual system, which in and of itself does raise challenges in relation to equality of services. There is a significant infrastructure disparity between privately funded and public health care service providers and given that the NHIS is intended to apply to both private and public sectors, there is need to develop a coordinated mechanism between the insurance schemes to ensure access to standardized quality of care.
(ii) Administrative capacity of NHIMA
Management of a universal health care scheme requires considerable human capital and expertise to manage the plethora of cases and claims, as well as process the reimbursements to private institutions for subsidized services.
(iii) Development of a health management system
An efficient health management system which includes a data base of all beneficiaries or members. As things stand the registration of beneficiaries is facilitate on an online platform which raises the question as to how people in rural and low income communities where there is low literacy and digitization are registered.
(iv) Limited access and coverage due to a lack of infrastructure
The concept of universal access and coverage operates on the premise that there are services to access in the first place and that a standardized package of benefits can be offered. This requires basic infrastructure, facilities, equipment and medicines. At the lowest end of the spectrum there are Zambians for whom the nearest health care facility is a distance of 500km with one doctor for every 12,000 patients (WHO:2018). Effective implementation of the NHIS therefore requires an improvement of the current health care system infrastructure.
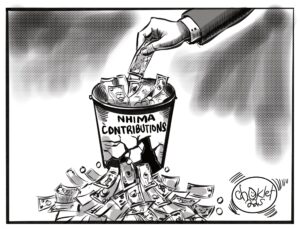
(v) Exclusion of informal sector
Although the NHIS contributions apply to both the formal and informal sector, tracking compliance by the informal sector is challenging due to a lack of documentation and formalization. The result is that an already overtaxed taxed base comprised of the formal sector shoulders the bulk of the costs in relation to the NHIS. The formal sector comprises less than 15 percent of the Zambian workforce (ILO:2018). Mass enrolment and participation of the informal sector is therefore necessary to mobilize resources and ensure equitable access and health care coverage.
Achieving universal health coverage is an ambitious and challenging feat, especially in the context of developing economies which have limited resources. It should be stated that NHIMA has made positive strides in terms of developing a Benefits Package which defines the services and products available to beneficiaries under the NHIS.
However, appropriate policies, sound governance and resource mobilization towards health financing can go a long way towards achieving quality health care for all.
Recommendations to achieve this include:
1) Investing in basic infrastructure, human resources/capital and financing systems;
2) Developing an effective health information system;
3) Implementing systems for procuring and distributing essential medicines, vaccines and technology, and
4) Expanding equitable access to comprehensive, quality, health care by expediting private sector engagement as a means of addressing infrastructure deficits across the health care system.
5) Developing initiatives to enhance enrolment of the informal sector and disenfranchised groups into the NHIS.
6) Strengthening multisectoral coordination to address the social determinants of health that ensure the sustainability of universal coverage.
7) Reviewing the legal framework in relation to the regulation of prudential requirements, competition, advertising, premiums, adverse selection and reporting requirements for private health insurance schemes in order to enhance the coexistence with the NHIS and the scale up of coverage
About the Author
Chileshe G. Mange is a Researcher at CTPD, an Advocate of the High Court for Zambia and a part-time tutor with the University of Zambia.