YES, you read that headline correctly. Zambia currently only has eight paediatric surgeons, and this is a great improvement. You see, when the current Zambia Association of Paediatric Surgery (ZAPS) president Dr Bruce Bvulani joined this field some years ago, he only had three seniors; two of whom have now passed and one has retired. So the fact that there are now eight fully trained Zambian paediatric surgeons and another 10 currently in training is exciting for Dr Bvulani, and it should excite us too, even if this is miles away from being adequate.
You see, our little humans are always at risk of injury or choking and in fact, Dr Bvulani, who is also UTH head of paediatric surgery, tells me that pulling out coins and other foreign objects from children’s throats or oesophagus is an every day occurrence. But that is not the only procedure paediatric surgeons do; they also engage in massive surgeries to correct birth defects like the separation of Siamese twins.
“At the moment we have eight Paediatric surgeons who are trained and then we have another about 8-10 in training. A couple of years ago, I was the only junior Paediatric surgeon and I had three other seniors who have since left the practice, two have passed and one has retired. So we have moved quite a bit in terms of increasing our numbers. We have a training programme which we call the Master of Medicine in Paediatric Surgery but we also have another local fellowship exam which is called the specialist training programme, STP, and then we also have a regional training programme which is under the college of surgeons of east, central and Southern Africa, the COSECSA, where you can also get the fellowship qualification. So through those means, we have managed to increase the number of surgeons,” Dr Bvulani says.
“We handle all kinds of conditions that children have. In the past, we used to also handle neurological diseases but with time, these have been taken over by the neurosurgeons and they are developing their own Paediatric neurosurgical specialty. Some of the things we have done are things like the separation of the Siamese twins which hit the news in 2018, Mapalo and Bupe, but everyday, there are so many surgical operations we do at UTH, at Arthur Davison Children’s Hospital in Ndola and at Levy Hospital where we have another centre. Our idea as Zambia Association of Paediatric Surgeons is to enhance the practice of Paediatric surgery in terms of capacity building, research and also, outside the hospital, we are trying to see how we can promote awareness of the surgical diseases that affect primarily children and how the community can help in dealing with those, awareness so that people can know what kind of diseases are there and issues which children can deal with such as for instance foreign body ingestion, on a daily basis we are removing coins from throats or oesophagus of children, so those are some of the areas that we want to go into. But also, there are some diseases which parents tend to keep at home which can be dealt with in the hospital where they think perhaps there’s no medical help.”
Asked what kind of conditions parents might be keeping at home not knowing there could be some help, Dr Bvulani said some neurological issues.
“There are conditions like neurosurgical diseases where a child has been born with a disability in the spine and perhaps they are not able to walk properly and over time, they develop issues of soiling and so on and parents may decide that this is just how this child is and they may not bring them forth to the hospital when there are possibilities of making that person’s life better. We may not be able to cure them in instances like that but we may be able to make their quality of life better. And parents may feel that they are the only ones who are experiencing such a thing but when they know that this is a disease that is out there, then it gives them more confidence to want to seek medical attention in situations like that,” he said.
“We do a lot of other operations, for instance umbilical hernia, when at the belly button there is a defect in the muscle and then there’s a protrusion which is common in girl children, we do repairs of those, and then lower down in the groin, there is what we call an inguinal hernia, you get a protrusion of contents inside the abdominal cavity outside. Those are the common procedures that we do but we have other procedures where we remove tumors, the common tumor that we remove is a kidney tumour, what’s called a Wilms tumour, it is a common tumour in Africa, probably the commonest tumour that you find with the abdomen in Africa and particularly here in Zambia and various other procedures that may not have to do with tumours like new born babies who are born with intestines that are not joined, these are also quite common so we have to do operations to join their intestines. We have various other things like where in boys testes haven’t come to the outside, and so we have to bring them out and stitch the defect, and also children born with abnormal or absent annal openings and so we do various procedures for that. I’m trying not to be too technical but there are also a lot of chest conditions that we deal with.”
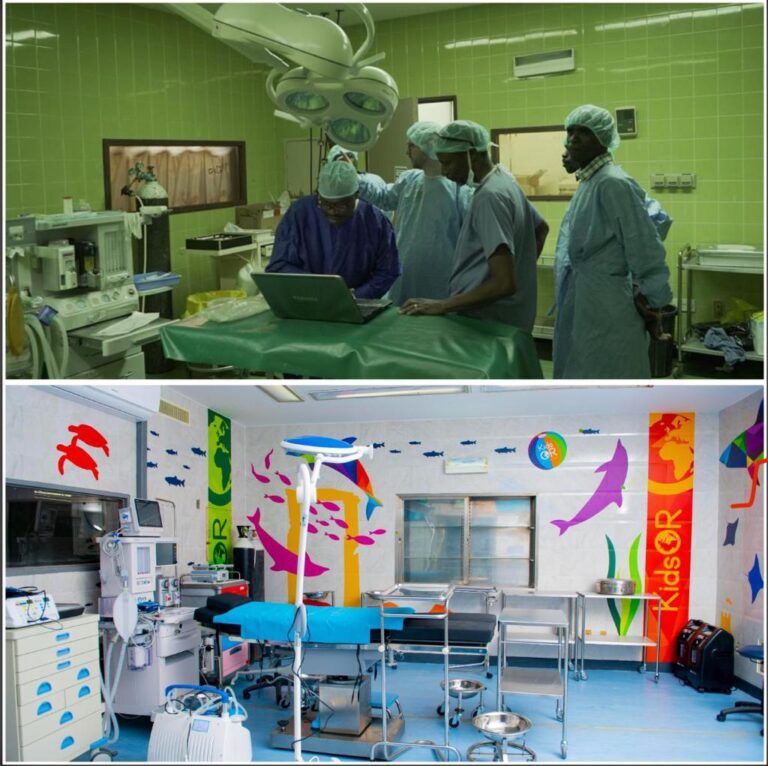
With all this amazing work that paediatric surgeons do, until 2021, they used to sometimes use adult-suited equipment on newborns and other tiny bodies, not to mention operating on these otherwise always happy souls in a very dull environment. KidsOR and Smile Train, however, changed this around when they invested over $300,000 (each) to refurbish several operating rooms for children around the country. Now, Dr Bvulani says even the health workers get a sense of joy as they work (see before and after pictures for UTH).
Dr Bvulani appealed to parents to be understanding if the surgeons asked them to wait for some time before surgery.
“With the increase in numbers of Paediatric surgeons, with our capacity but also with the refurbishment of our theaters, we’re able to do more than we were able to do before, so we have reduced quite a number of the burden so people shouldn’t be afraid to come and approach the facilities. But as always, it is always difficult to juggle between the more important cases and the one that can wait. So you might find that sometime you’ll find that we’ll ask you to hold on for something that may take a few more months and may not cause damage to the child and can wait for another two months compared to say something that needs to be done immediately. For instance, if someone has a growing mass which can cause death, we would deal with that rather than a swelling which one can have for another few months so they need to just bear with us when they come,” said Dr Bvulani.
“And for those mothers whose children have conditions which they’d feel perhaps there’s no help or conditions which they feel they have not seen anyone deal with it, they should feel free to come and see us at UTH, they can visit us at D-Block or come to the Children’s Hospital and they will be redirected or indeed they can come to the Arthur Davies Children’s Hospital in Ndola or Levy Hospital and look for the Paediatric surgeon who is there and then in the near future, other sites will be opened up as well and then we’ll let you know if where that is so we are there to help you and we’re ready to help you. We’re looking forward to having them come and visit us.”
Meanwhile, Kids OR Africa Director Rosemary Mugwe said her organisation had done a lot of work in Zambia because there’s political will and the environment is enabling.
“In Zambia, we have the biggest programme in the sub-saharan region. So, we have three operating rooms at the University Teaching Hospitals, all fully equipped…we have also done the same for Arthur Davidson Children’s Hospital in Ndola, three of them also, one in partnership with Smile Train. We have also gone ahead and implemented a similar project at the Kabwe Hospital and at Chipata. As we speak right now, we have a shipment coming in for Livingstone Hospital. In the pipeline, we also have Kitwe. It’s been a country that we have had a lot of investment, there’s political will and the environment is enabling,” said Mugwe.
“We’re also sponsoring five trainee paediatric surgeons, one completed last year and was employed at UTH and we have four in training…health is a human right, access to surgery when you need it is a human right. Children take up 45 to 50 per cent of the population in each country in sub-saharan Africa so it is so sad to find a child who just had a broken leg while playing live with a lifelong disability because they cannot access that timely surgery when it is needed.”